Behavioural Challenges
Practical strategies that can improve communication and interaction with a person with dementia
Introduction
Supporting a family member with dementia can pose challenges for the carer and extended family. People with dementia have a progressive brain disorder that makes it increasingly difficult for the person to remember things, think clearly, communicate with others, or manage activities of daily living. In addition, dementia may cause mood swings and even change a person’s personality and behaviour. This Fact Sheet provides some practical strategies for dealing with the behaviour concerns and communication difficulties encountered when caring for a person with dementia.
Ten Tips for Communicating with a Person with Dementia
We are not born knowing how to communicate with a person with dementia, but we can learn. Improving communication skills can make caregiving less stressful and improve the quality of your relationship with your family member. Good communication skills also improve your ability to cope with and prevent problem behaviours you may encounter as you support a person living with dementia.
Set a positive mood for interaction. Your attitude and body language communicate your feelings and thoughts more strongly than your words. Set a positive mood by speaking to the person with dementia in a pleasant and respectful manner. Use facial expressions, tone of voice and physical touch to help convey your message and show your feelings of affection.
Get the person’s attention. Limit distractions and noise e.g. turn off the radio or TV, close the curtains, shut the door, or move to quieter surroundings. Before speaking, make sure you have his/her attention; address the person by name, identify yourself by name and your relationship, and use nonverbal cues and touch to help keep the person focused. If the person is seated or lying, get down to their level and maintain eye contact.
State your message clearly. Use simple words and sentences. Speak slowly, distinctly and in a reassuring tone. Pitch your voice low and at an average volume. If s/he doesn’t understand the first time, use the same wording to repeat your message or question. If the person still doesn’t understand, wait a few minutes and rephrase the question. Try not to raise your voice in volume or pitch. Use the names of people and places instead of pronouns or abbreviations, and be specific. For example, use the phrase “Sue will be bringing groceries at noon.” rather than “She’ll drop by around lunch.“
Listen with your ears, eyes and heart. Be patient in waiting for your family member’s reply. If s/he is struggling for an answer, it’s okay to suggest words. Watch for nonverbal cues and body language, and respond appropriately. Always strive to listen for the meaning and feelings that underlie the words.
Break down activities into a series of steps. This makes many tasks much more manageable. Encourage your family member to do what s/he can, gently reminding him/her of steps that need to be taken and assisting with steps s/he is no longer able to accomplish alone. Visual cues, such as showing the person with your hand where to place the dinner plate, can be very helpful.
When the going gets tough, distract and redirect. When your family member becomes upset, try changing the subject or the environment. For example, ask him/her for help or suggest going for a walk. It is important to connect with the person on a feeling level, before you redirect. You might say, “I see you’re feeling sad - I’m sorry you’re upset. Let’s go get something to eat.“
Respond with affection and reassurance. People with dementia often feel anxious and unsure of and recall things that never really occurred. Avoid trying to convince them they are wrong. Stay focused on the feelings they are demonstrating (which are real) and respond with verbal and physical expressions of comfort, support and reassurance. Sometimes holding hands, touching, hugging and praise will get the person to respond when all else fails.
Remember the good old days. Remembering the past is often a soothing and affirming activity. Many people with dementia may not remember what happened 45 minutes ago, but can clearly recall their lives 45 years earlier. Therefore, avoid asking questions that rely on short-term memory, such as what they had for lunch. Instead, try asking general questions about the person’s distant past, as this information is more likely to be retained.
Maintain your sense of humour. Use humour whenever possible, though not at the person’s expense. People with dementia tend to retain their social skills and usually laugh along with you.
Strategies to improve interaction
Personality and behaviour change are perhaps the greatest challenges of caring for someone with dementia. To manage these challenges you will need creativity, flexibility, patience and compassion. It helps to not take things personally and maintain your sense of humour.
To start, consider these ground rules:
We cannot change the person. Dementia is a brain disorder that shapes the way a person behaves. When you try to control or change his/her behaviour, you’ll most likely be unsuccessful or be met with resistance. It’s important to:
Try to accommodate, not control, the behaviour. For example, if the person insists on sleeping on the floor, place a mattress on the floor to make him more comfortable.
Remember that we can change our behaviour or the physical environment. Changing our own behaviour will often result in a change in our family member’s behaviour.
Check with the doctor first. There may be an underlying medical reason for behavioural problems. Perhaps the person is in pain or experiencing an adverse side effect from medication. In some cases, like incontinence or hallucinations, a medical treatment might assist in managing the problem.
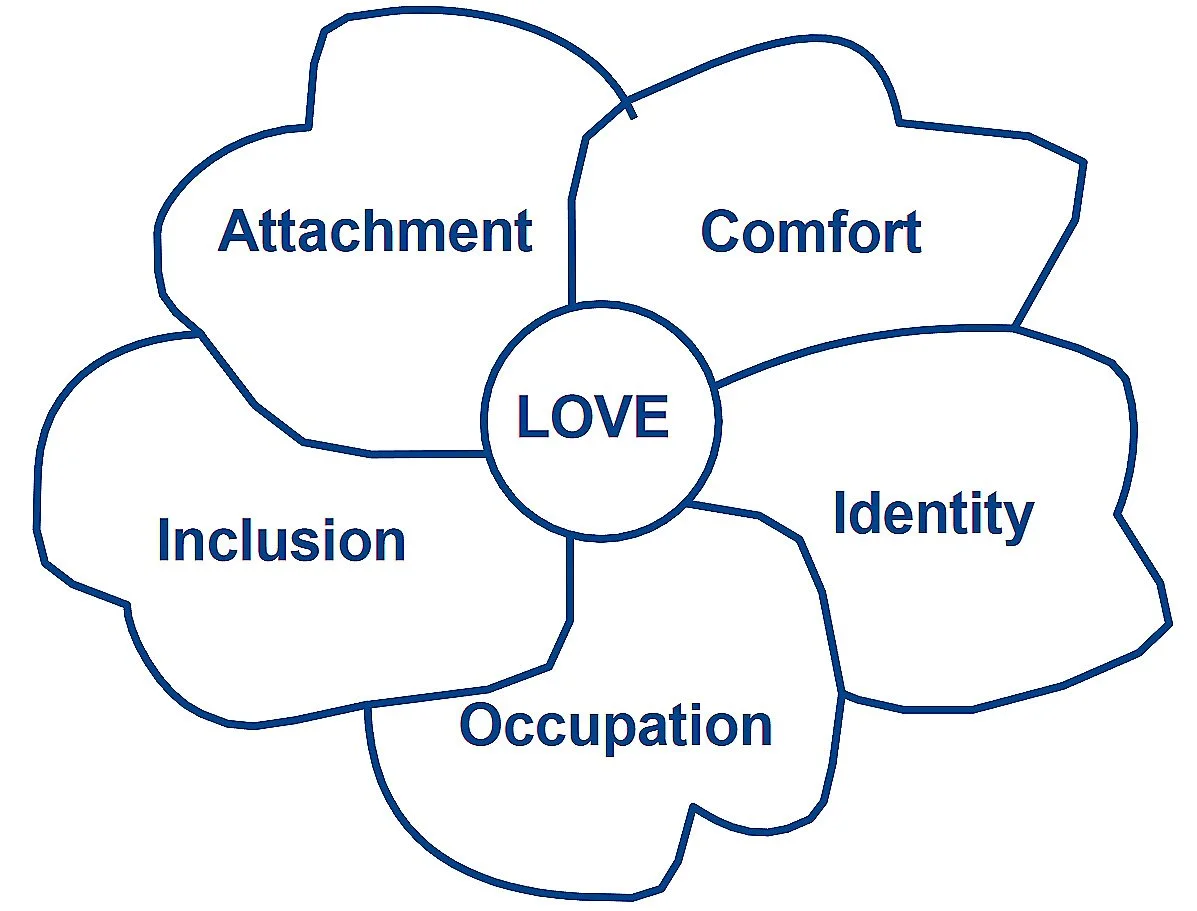
Behaviour has a purpose. People with more advanced dementia typically cannot tell us what they want or need. For example, they might take all the clothes out of the closet on a daily basis, and we wonder why. Perhaps the person is fulfilling a need to be busy and productive. Always consider what need the person might be trying to meet with their behaviour—and, when possible, try to accommodate them. Professor Thomas Kitwood recognised that all people have basic psychological needs, and behaviour (the way we all act) is related to getting our needs met in these areas. He created a “flower” to explain the psychological needs of all people, as below:
Psychological needs
Behaviour is triggered. It is important to understand that behaviour is triggered—it doesn’t occur out of the blue. Something a person did or said might have triggered a behaviour in response, or it could be a change in the physical environment, such as familiar things having been moved. The root to changing behaviour is disrupting the patterns that we create. Try a different approach such as not insisting someone gets up for breakfast or giving them something meaningful to do to avoid boredom.
What works today, may not work tomorrow. The multiple factors that influence troubling behaviours and the natural progression of the disease process means that solutions that are effective today may need to be modified tomorrow—or may no longer work at all. The key to managing difficult behaviours is being creative and flexible in your strategies to address a given issue.
Get support from others. You are not alone—there are many others caring for someone with dementia. Locate your nearest Dementia NZ organisation, or call 0800 4 DEMENTIA to be connected with someone who can help.